Education
Ph.D.
M.Sc.
B.A.Sc. Honors
B.Sc.
'04-'06
'02-'04
'97-'02
'14-'17
Queen's University - School of Computing
Supervised by Dr. Stewart
Image Guided Catheter Ablation: Error Compensation
Queen's University - School of Computing
Supervised by Dr. Stewart & Dr. Kunz
Computer Assisted Mosaic Arthroplasty – A Bone Model Trial
Queen's University - Electrical & Computer Engineering
Monte-Carlo Simulations in Parallel Processing on CellBE
Supervised by Dr. Afsahi and Dr. Ryan Grant
Queen's University - Physics
Research Project on Neural Networks
St Lawrence College - fine woodworking certificate
Employment History
'21-present
'09-present
'19-21
'16-19
'08-17
'12-15
'10
'09
'07-09
Senior System Solution Specialist
Queen's University
Researcher
Queen's University
Instructional Designer MultiMedia Analyst
Queen's University
Learning System Manager
Queen's University
Teaching Assistant & Fellow/Adjunct Professor/Lab Instructor
Queen's University, Royal Canadian Military College
Software Developer Engineer
ESG Solutions
NSERC CREATE - researcher
Queen's University - Mechanical Engineering
supervised by Dr. Kevin Deluzio and Scott Grant
NSERC USRA - researcher
Royal Canadian Military College
supervised by Dr. Chaudry
SWEP - undergraduate researcher
Queen's University - Ongwanada
supervised by Dr. Holden
Research
5D+ Patient Specific Cardiac Models
A significant part of my research has been on time-varying models of the heart. So what do I mean by 5D+?
2D and 3D modelling of cardiac anatomy is quite prevalent. Usually, 3D is created from CT/MR volumetric data or from electrophysiology catheters. It’s also possible (with less resolution) using ultrasound. 2D imaging is often fluoroscopic radiological visualization.
For the most part, these models are static or the movement is treated as an artifact in the imaging modality. This works fine for anatomy that doesn’t move much (see my orthopaedic work in the CAMA tab).
The heart is uniquely complicated. It moves (and if it’s not, find a different doctor). It also has two types of forces driving its movement: respiratory and cardiac (pulse).
To complicate things even more, these movements are at different magnitudes and frequencies (hearts beat much faster than your breathing cycle). And usually the people who need heart surgeries don’t have hearts that behave in a consistent and predictable fashion.
Below is an atrial fibrillation patient-specific model of a left atrium generated by my computer modelling software that can visualize cardiac movement in real-time based on prior patient data.
But if this were not complicated enough, heart surgery has another dimension to the problem. In the above model, we looked at the heart as a mechanical device — but what drives it?
The heart also has an electrical component. Electrical signals are a critical aspect of cardiac mechanical behavior. In the model below, I superimposed the voltage activation pattern (i.e., electrical activity) onto the dynamic model.
This is where the 5D+ comes from: 3D position, plus two distinct forces that change over time (making 5D), plus (+) the electrical activity.
One might ask, “Why is this research important?” Cardiac disease is the largest source of death in the world. The initial motivation for this research was to help guide surgical tools to treat cardiac arrhythmias. Arrhythmias are a spectrum of conditions manifesting in the heart beating too rapidly (tachycardia), too slowly (bradycardia), or irregularly.
Arrhythmias can lead to thromboembolic events and congestive heart failure. The consequences can be debilitating or deadly. Current treatments range from noninvasive strategies (pharmacological therapy, which can strain the kidney and liver) to minimally invasive techniques (catheter-based ablation) to extensive open-heart surgical techniques.
With this in mind, catheter ablation can be a more definitive solution than pharmacological intervention without the significant risks of open surgery. However, the procedure comes with challenges in navigating the heart without direct line of sight. At the moment, this is done with a static 3D model — but preliminary results of this research show that the approach I developed is about 6× more accurate than leading manually constructed (and automated) models, with significantly less variance. Thus, if a surgeon is trying to ablate and isolate an aberrant signal or excise a tumor, this visualization is more likely to reflect true anatomy and should yield better outcomes.
Instrument Recovery
Part of my PhD research work focused on developing an approach for catheter position and pose recovery in a distorted field.
Motivation & Challenges
EAM systems can be prone to misalignment (progressive and spontaneous), which we have colloquially termed “drift” and “shift”. In other words, the reference origin can move spontaneously or progressively from its previous position. From a user’s perspective, this can appear as if the instruments are in a different position in the heart (e.g., at one instant the catheter could be positioned inside the heart, and the next it appears outside the heart altogether).
At present, the operator’s sole recourse is to reset the system, which requires remapping the endocardium and results in loss of previous data (electro-anatomic map and ablation points). This is highly undesirable.
Preliminary Work
This research is still in progress.
Computer Assisted Mosaic Arthroplasty
Osteoarthritis is the most common form of arthritis and a degenerative joint disease. Cartilage in joints does not naturally recover quickly once damaged (due to injury or “wear and tear”). It is generally painful, and the common long-term practice is joint replacement (often reserved for older patients since artificial joints have a limited lifespan).
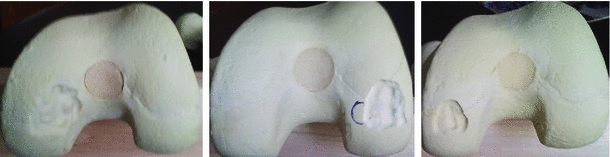
An alternative is mosaic arthroplasty (osteochondral implantation). In this procedure, the orthopaedic surgeon harvests joint cartilage from non-load-bearing parts of the joint and implants them at the damage site (the lesion) — analogous to filling a pothole.
Traditional mosaic arthroplasty is difficult: the surgeon must recreate the original joint surface near perfectly. If they insert plugs too high/proud, they shear off. If too shallow, the defect can fill with less desirable fibrocartilage instead of articular cartilage. If too large a gap is left below the plug, it can fill with fluid and form a cyst-like structure.
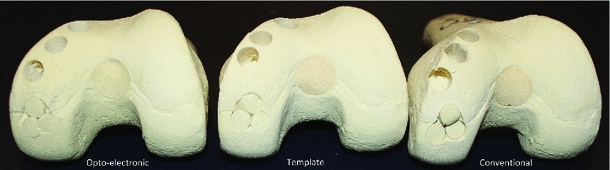
Computer intervention removes much of the human error and guesswork. My (collaborative) work has taken two forms: (1) thermoplastic custom 3D-printed templates (customized jigs), and (2) opto-electronic tracking of surgical tools.
Initial Step
The initial step is acquiring preoperative diagnostic CT (or MR) and segmenting the joint. Segmentation can be achieved semi-automatically using thresholding, edge detection, and region growing methods, but the region of interest (the lesion) is typically manually segmented (or edited). The patient’s ideal curvature is recreated by consultation with the surgeon using a manual planner (Dr. Kunz and others) or planning software (originally designed by Dr. Jiro Inoue, PhD). Using the reconstructed joint, surgical sites are planned.
Method 1 - Custom Template Guides
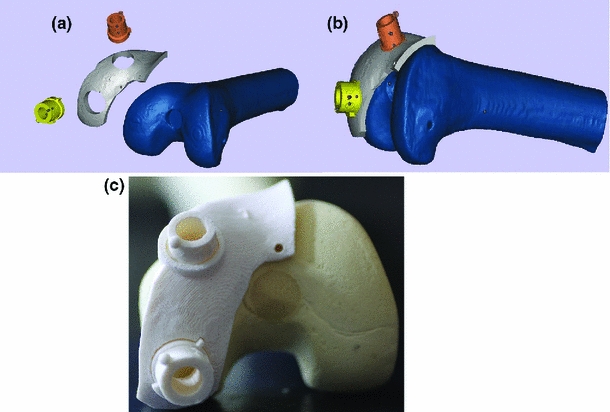
One approach uses thermo-plastic templates. Using reconstructed patient knee models, surgical sites are planned and used to design thermoplastic templates that are 3D-printed. These templates fit the patient’s joint and guide the surgical instrument from harvest to recipient site (accounting for 6 degrees of freedom).
My work showed this method to be significantly more accurate (in customized bone models) than the conventional procedure, with reduced variance. The shortcoming is that it requires a more invasive opening of the joint cavity compared to the opto-electronic method.
Method 2 - Optical Electronic Guidance
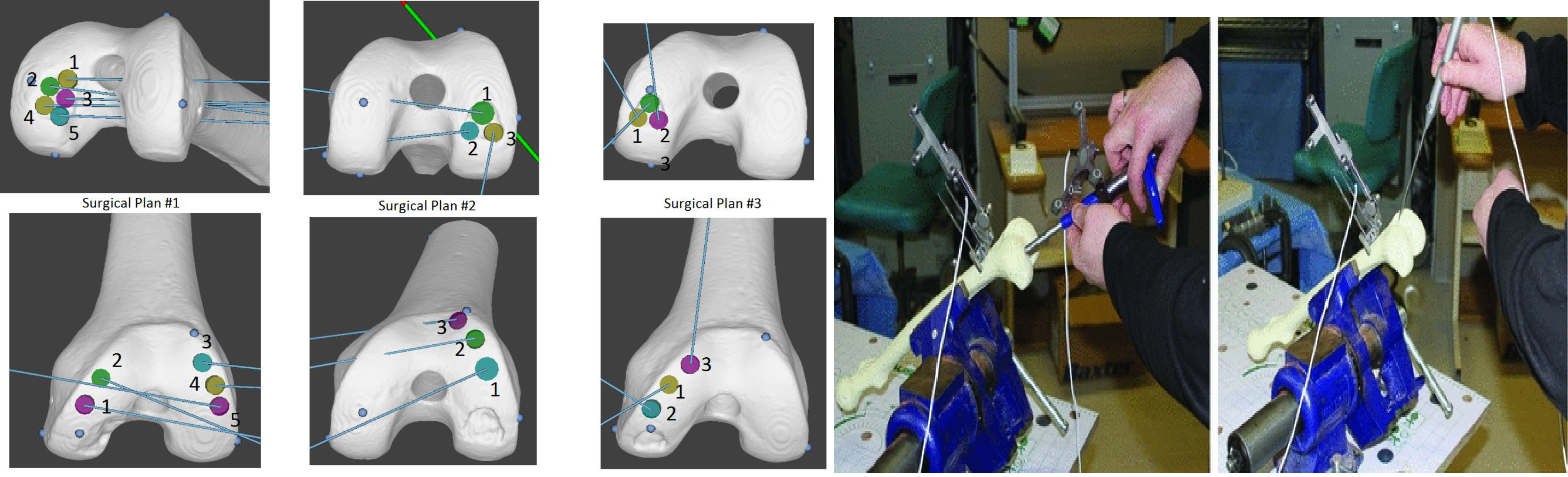
The other method involves attaching optical LED markers and tracking instruments using a stereoscopic camera (analogous to tracking used in motion-gaming systems, but with significantly greater reliability and accuracy). The surgical plan is overlaid on the patient’s model. The system is calibrated using 3D-printed and machined calibration blocks. Then, using an ICP-variant, the patient’s joint is registered with the computational model. The navigation system tracks instruments relative to the joint surface, providing visual feedback (6 DOF) to the surgeon.
This process is significantly more accurate than the conventional procedure and only marginally less accurate than the template method. It is more time-consuming due to calibration/registration steps, but has the advantage of being usable in less-invasive arthroscopic variants.
Validation
More Detailed Reading
Sebastyan, S., Kunz, M., Stewart, A. J., & Bardana, D. D. (2015). Image-guided techniques improve accuracy of mosaic arthroplasty. International Journal of Computer Assisted Radiology and Surgery. LINKED HERE
Sebastyan, S. (2013). Computer-assisted mosaic arthroplasty: A femur model trial. LINKED HERE
Teaching
Mathematics
- Calculus (differentiable, intregral, multivariate)
- Differential equations
- Graph theory
- Game theory
- Statistics
- Probability
- Fourier Transforms
- Linear Algebra
Data Stuctures & Algorithms
- Sorting & Searching
- Gradient Descent
- Data structures
Scientific Computing and Data Analysis
- PCA
- SVD
Coordinate Transformation
- Basic coordinate transformationsg
- ICP
- Quaternions
- Coherent Point Drift
Interpolations & Shape Change Models
- Level Set Methods
- ICP
- Quaternions
- Coherent Point Drift
Sports & Coaching
Hockey
I played at The Taft School (Watertown, CT) and before that at the rep/AAA level and Loyola High School .
I coached over a dozen teams (ranging from Rep to house league) and have run skill development camps for the last 4 years.
Baseball
I played Junior AA baseball up to age 21 and currently coach the Kingston Thunder Rep team. Also commissioner for the house league division.
Football
I played collegiate football and played inside linebacker for the McGill Redmen.
Martial Arts
- Kru (equivalent of black belt) in Muay Thai
- black belt in SAW
- black belt in Pankration
- brown belt in Judo
- level 1 Combat Sambo
Hobbies
SCUBA
I have my advanced and master PADI SCUBA certificate and enjoy diving and snorkelling when travelling (including, Fiji, Mexico and Jamaica)
Woodworking
I'm a certified gold seal Woodworking and Fine Furniture graduate of St Lawrence College. I've built my share of furniture around my house.









